Table of Contents
Introduction
In recent weeks, outbreaks of Human Metapneumovirus (hMPV) have been reported in countries such as China and India, raising significant public health concerns. As a common yet often underestimated respiratory pathogen, hMPV primarily affects children, the elderly, and individuals with weakened immune systems. Its sudden rise in cases highlights the need for increased awareness about its transmission, symptoms, treatment options, and prevention strategies. In this article, we delve into the key aspects of hMPV to help you better understand and mitigate the risks associated with this virus.
Human metapneumovirus (HMPV) is a significant yet often overlooked respiratory virus that can lead to a range of illnesses, particularly in vulnerable populations such as young children, the elderly, and individuals with weakened immune systems. Although it was first identified in 2001, awareness and understanding of HMPV have grown, highlighting its potential to cause serious respiratory infections similar to those caused by more well-known viruses like influenza and respiratory syncytial virus (RSV).

Currently, there is no specific antiviral treatment or vaccine available for HMPV, which underscores the importance of preventive measures. Good hygiene practices—such as frequent handwashing, avoiding close contact with sick individuals, and maintaining clean surfaces—are essential in reducing the spread of this virus. As we continue to navigate the complexities of respiratory infections, understanding HMPV’s transmission modes, symptoms, treatment options, and prevention strategies is vital for protecting public health and ensuring better outcomes for those affected.
What Are the Main Transmission Modes of Human Metapneumovirus?
Understanding these transmission modes is crucial for implementing effective prevention strategies and reducing the spread of HMPV, particularly in high-risk populations.
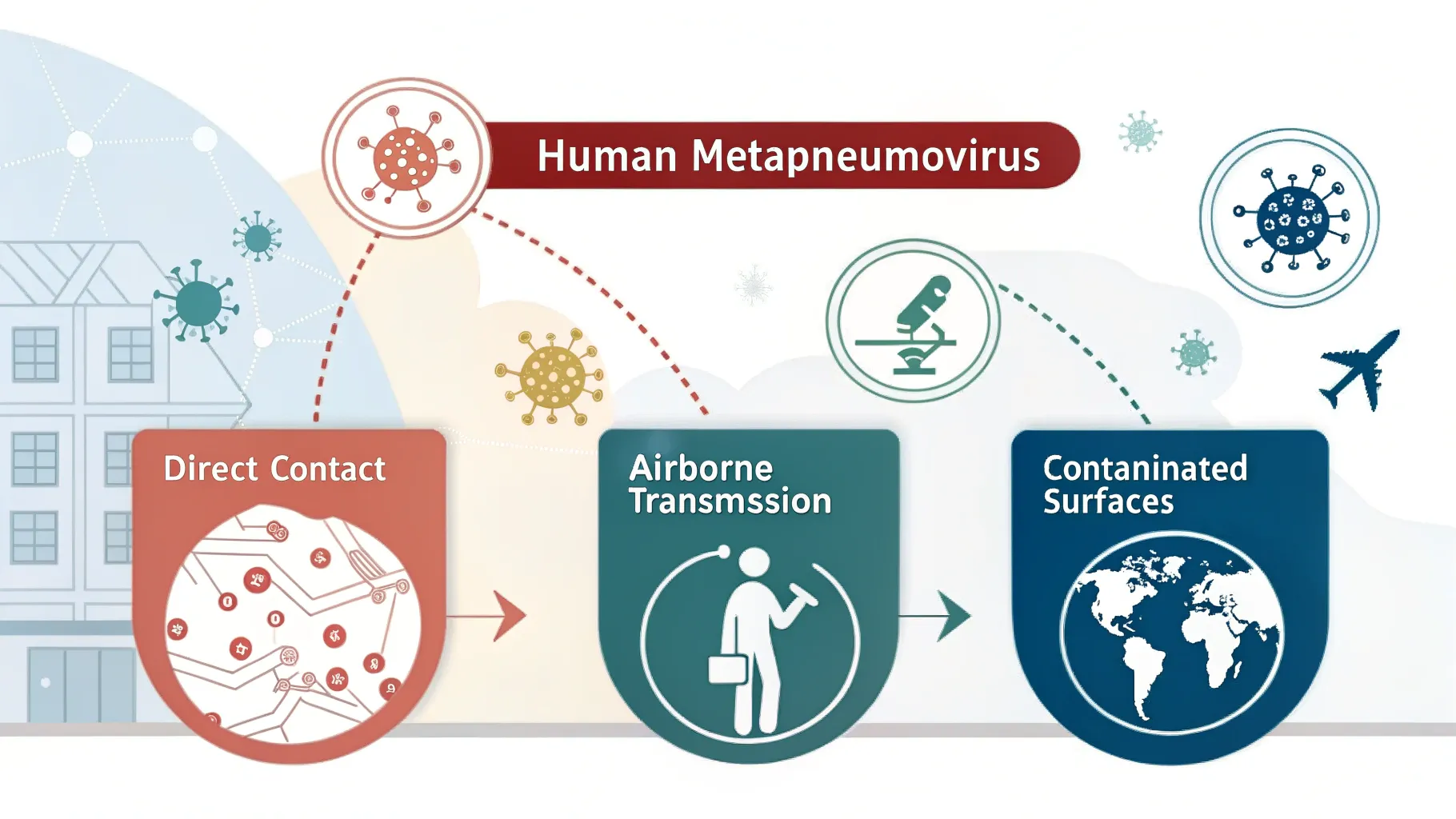
Direct Contact
HMPV can be transmitted through direct contact with an infected individual. This includes actions such as kissing, touching, or shaking hands with someone who is infected. The virus can be present in respiratory secretions, making close interactions a significant risk factor for transmission.
Airborne Transmission
Airborne transmission occurs when an infected person coughs or sneezes, releasing respiratory droplets that contain the virus into the air. These droplets can be inhaled by others nearby, facilitating the spread of HMPV in crowded or enclosed spaces.
Contaminated Surfaces
The virus can also survive on surfaces for several hours. If a person touches a contaminated surface and subsequently touches their face—especially the eyes, nose, or mouth—they can become infected. This mode of transmission underscores the importance of maintaining good hygiene practices to minimize risk.
| Method | Speed | Examples | Insight |
|---|---|---|---|
| Direct Contact | Rapid | Kissing, touching | High risk for HMPV spread. |
| Airborne | Quick | Coughing, sneezing | Spreads in crowded spaces. |
| Surfaces | Slower | Touching surfaces | Can survive on surfaces for hours. |
In summary, while direct contact and airborne transmission of HMPV occur rapidly—often within seconds to minutes—contaminated surface transmission tends to be slower but still poses a significant risk due to the virus’s ability to survive on surfaces.
Common Symptoms of Human Metapneumovirus Infection
Human metapneumovirus (HMPV) infection can present a range of symptoms that vary in severity between individuals, particularly when comparing children and adults. Here’s an overview of the common symptoms associated with HMPV:
Respiratory Symptoms
- Cough: A persistent cough is one of the most common symptoms, often resembling that seen in a cold or other respiratory infections.
- Nasal Congestion: Patients frequently experience a runny or stuffy nose.
- Sore Throat: This symptom is common and contributes to the overall discomfort during infection.
- Fever: Fever is reported in many cases, particularly among children, and can be a significant indicator of HMPV infection.
- Wheezing and Shortness of Breath: In more severe cases, especially in young children or those with pre-existing conditions, wheezing and difficulty breathing may occur, indicating lower respiratory tract involvement.
Systemic Symptoms
- Fatigue: General tiredness is common during viral infections, including HMPV.
- Gastrointestinal Symptoms: Nausea, vomiting, and diarrhea have also been reported but are less common than respiratory symptoms. These may occur in conjunction with other symptoms.
Symptoms in Children vs. Adults
- Children: HMPV is particularly prevalent in young children, especially those under 5 years old. Symptoms often include typical upper respiratory signs like cough and fever. However, they are also at risk for more severe complications such as bronchiolitis and pneumonia. Studies indicate that 5% to 16% of infected children may require hospitalization due to severe symptoms.
- Adults: While adults may experience similar upper respiratory symptoms, they are more likely to develop complications such as viral pneumonia or exacerbations of chronic conditions like asthma or chronic obstructive pulmonary disease (COPD). Adults over 65 or those with weakened immune systems are at higher risk for severe illness.

Effective Treatment Methods for Human Metapneumovirus
Effective treatment for Human Metapneumovirus (HMPV) primarily focuses on alleviating symptoms, as there is currently no specific antiviral therapy approved for this infection.
How is human metapneumovirus treated?
There aren’t any antiviral medications that treat human metapneumovirus. Most people can manage their symptoms at home until they feel better.
If you or your child are severely ill, you might need to be admitted to the hospital. There, healthcare providers can monitor your condition and help prevent you from getting sicker. They might treat you with:
- Oxygen therapy. If you’re having a hard time breathing, a provider may give you extra oxygen through a tube in your nose or mask on your face.
- IV fluids. Fluids delivered directly to your vein (IV) can keep you hydrated.
- Corticosteroids. Steroids can reduce inflammation and might ease some of your symptoms.
Do you need antibiotics for human metapneumovirus?
No. Antibiotics only treat bacteria. Since HMPV is a virus, antibiotics won’t get rid of it. Sometimes people who get pneumonia from HMPV also get a bacterial infection at the same time (secondary infection). If your provider prescribes antibiotics, it would be to treat any secondary infections.

How to Prevent Human Metapneumovirus Infection
To effectively prevent Human Metapneumovirus (HMPV) infection, several strategies can be implemented, focusing on hygiene practices, avoiding crowded places, and the current lack of a vaccine. Here’s a detailed overview:
Vaccination
- Current Status: As of now, there is no vaccine specifically available for HMPV. This highlights the importance of relying on other preventive measures to reduce the risk of infection.
Hygiene Practices
- Hand Hygiene: Regular handwashing with soap and water for at least 20 seconds is crucial. If soap and water are unavailable, alcohol-based hand sanitizers can be used. This practice helps eliminate the virus from hands, especially after touching potentially contaminated surfaces or before touching the face.
- Respiratory Etiquette: Covering the mouth and nose with a tissue or elbow when coughing or sneezing can prevent the spread of respiratory droplets that may contain the virus. Disposing of tissues properly and washing hands afterward is essential.
- Avoid Touching Face: Avoiding contact with the eyes, nose, and mouth with unwashed hands can significantly reduce the risk of infection.
- Cleaning Surfaces: Regularly disinfecting frequently-touched surfaces (like doorknobs, light switches, and mobile devices) can help eliminate any viral presence in shared environments.
Avoiding Crowded Places
- Social Distancing: Staying away from crowded areas, especially during peak respiratory virus seasons (late winter and early spring), can minimize exposure to HMPV and other respiratory pathogens. This is particularly important for individuals at higher risk, such as young children and the elderly.
- Staying Home When Sick: Individuals exhibiting symptoms of respiratory illness should remain at home to prevent spreading the virus to others.

Seasonality and High-Risk Groups of Human Metapneumovirus
Human Metapneumovirus (HMPV) exhibits distinct seasonal trends and affects various high-risk populations. Here’s a detailed overview based on the latest findings:
Seasonal Trends
- Peak Seasons: HMPV infections typically peak during late winter and spring. Surveillance data from the CDC indicates that in temperate climates, HMPV activity often begins in winter and can last through spring, with significant peaks observed from December to March.
- Biennial Patterns: Some studies have noted a biennial pattern of HMPV incidence, where alternating years show significant variations in infection rates. For instance, a study conducted from 2011 to 2016 documented four epidemic periods with peaks occurring every other year.
- Geographical Variations: The timing of peaks can vary by region. For example, in subtropical areas like Hong Kong, higher HMPV activity has been recorded during spring and early summer, contrasting with the winter peaks seen in temperate regions.
High-Risk Populations
- Young Children: HMPV is particularly prevalent among young children, especially those under the age of 5. Studies show that a significant portion of infections occurs in this demographic, with many requiring hospitalization due to severe respiratory symptoms.
- Elderly and Immunocompromised Individuals: Older adults and individuals with weakened immune systems are also at increased risk for severe illness from HMPV. The infection can exacerbate existing health conditions, leading to complications such as pneumonia.
Impact of Age and Health Status
- Age Factor: Young children are more susceptible to severe outcomes from HMPV infection due to their developing immune systems. Research indicates that up to 78% of HMPV-positive cases occur in children younger than three years old.
- Health Status: Individuals with pre-existing respiratory conditions (such as asthma or chronic obstructive pulmonary disease) face a higher risk of complications when infected with HMPV. The presence of other respiratory viruses during peak seasons can further complicate health outcomes, contributing to increased healthcare utilization during winter months.